What is a Slipped disc?
 |
| Slipped Disc |
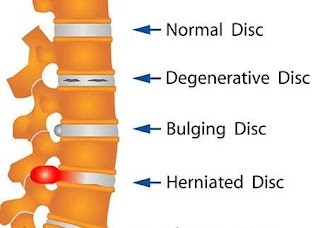
A slipped disc, also known as a herniated or prolapsed disc, is a condition that occurs when one of the spinal discs in your back ruptures or bulges out of its normal position. The spinal discs are the soft, gel-like cushions that sit between the vertebrae, or bones, of your spine. They help absorb shock and provide flexibility to the spine.
When a disc slips out of place, it can press against the surrounding nerves or spinal cord, causing pain, numbness, or weakness in the affected area. This can occur in the neck, middle back, or lower back.
Slipped discs can be caused by a variety of factors, including age-related wear and tear, injury, poor posture, and repetitive strain. Treatment options may include rest, pain relief medication, physical therapy, and in severe cases, surgery.
Related Anatomy
The spine is made up of a series of bones called vertebrae, which are separated by intervertebral discs. Each disc is made up of a tough outer layer called the annulus fibrosus, and a soft, gel-like center called the nucleus pulposus. The spinal cord runs through a central canal formed by the vertebrae, and it is surrounded and protected by the meninges, which are three layers of protective tissue.
There are 33 individual vertebrae in the human spine, divided into five regions: cervical (neck), thoracic (upper back), lumbar (lower back), sacral (pelvic), and coccygeal (tailbone). Each region has a different number of vertebrae and a slightly different shape and function.
The spinal nerves branch out from the spinal cord through spaces between the vertebrae, and they are responsible for transmitting sensory and motor signals to and from different parts of the body. The spinal discs help cushion the vertebrae and absorb shock, while also allowing for movement and flexibility in the spine.
Causes of Slipped disc
The causes of a slipped disc can be diverse, and in many cases, it is a result of a combination of factors. Some common causes include:
- Age-related degeneration: The spinal discs lose water content and elasticity with age, making them more prone to rupture or herniate.
- Trauma or injury: An injury or trauma to the spine, such as a fall, can cause a slipped disc.
- Poor posture: Sitting or standing in a poor posture for extended periods can put excessive pressure on the spinal discs, leading to disc herniation.
- Repetitive strain: Repetitive activities such as lifting heavy weights, bending, twisting, or carrying out tasks that require repetitive movement can put strain on the spinal discs.
- Genetics: Some people may be more susceptible to disc degeneration due to genetic factors.
- Smoking: Smoking can damage the spinal discs and reduce their ability to absorb shock.
- Obesity: Excess body weight can put more pressure on the spinal discs, increasing the risk of herniation.
- Occupation: People who work in jobs that require heavy lifting or prolonged sitting may be at a higher risk of developing a slipped disc.
It is essential to seek medical attention if you experience symptoms of a slipped disc, as early diagnosis and treatment can help prevent further damage to the spine.
Symptoms of slipped disc
A slipped disc, also known as a herniated or prolapsed disc, can cause a range of symptoms depending on the severity and location of the disc problem. Some common symptoms include:
- Back pain: This is the most common symptom of a slipped disc, particularly in the lower back. The pain may be sudden or gradual and can range from mild to severe.
- Sciatica: When a slipped disc presses against a nerve, it can cause pain, numbness, and tingling in the legs. This is known as sciatica, and it usually affects only one leg.
- Muscle weakness: A slipped disc can cause muscle weakness, particularly in the legs or feet, making it difficult to walk or stand.
- Reduced range of motion: If a slipped disc is affecting the mobility of the spine, it can cause stiffness and reduced range of motion.
- Bowel or bladder problems: In rare cases, a slipped disc can cause bowel or bladder problems, including difficulty controlling bowel or bladder function.
It's important to note that not everyone with a slipped disc will experience symptoms, and some people may experience only mild symptoms that resolve on their own. However, if you experience any of the above symptoms, it's important to see a doctor for an accurate diagnosis and appropriate treatment.
Risk factor for slipped disc
Several risk factors can increase the likelihood of developing a slipped disc, including:
- Age: As we age, the discs in our spine can become weaker, making them more prone to damage and herniation.
- Occupation: Jobs that involve heavy lifting, twisting, or repetitive bending can increase the risk of a slipped disc.
- Genetics: Some people may inherit a predisposition to developing a slipped disc.
- Weight: Being overweight or obese can put extra strain on the spine and increase the risk of a slipped disc.
- Smoking: Smoking can reduce the blood supply to the discs in the spine, making them more susceptible to damage.
- Poor posture: Poor posture can put extra strain on the spine and increase the risk of a slipped disc.
- Previous back injury: If you've had a back injury in the past, you may be more likely to develop a slipped disc.
It's important to note that having one or more of these risk factors does not necessarily mean that you will develop a slipped disc, and some people may develop a slipped disc without any known risk factors. However, if you have one or more of these risk factors, it's important to take steps to protect your back, such as maintaining a healthy weight, practicing good posture, and avoiding heavy lifting or other activities that can strain the back.
Differential Diagnosis
Differential diagnosis is a process of determining the possible medical conditions or diseases that may be causing a patient's symptoms. It involves considering various factors such as the patient's medical history, physical examination, laboratory tests, imaging studies, and other relevant information to arrive at a diagnosis. Here are some examples of differential diagnoses for common symptoms:
- Chest pain:
- Heart attack
- Angina
- Gastroesophageal reflux disease (GERD)
- Pneumonia
- Pulmonary embolism
- Headache:
- Migraine
- Tension headache
- Cluster headache
- Sinusitis
- Brain tumor
- Abdominal pain:
- Appendicitis
- Gallstones
- Gastroenteritis
- Pancreatitis
- Ulcerative colitis
- Joint pain:
- Lumbar Spondylosis
- Rheumatoid arthritis
- Gout
- Lupus
- Fibromyalgia
It's important to note that this is not an exhaustive list, and there can be many other possible conditions that may cause these symptoms. A healthcare provider will need to perform a thorough evaluation to arrive at an accurate diagnosis and develop an appropriate treatment plan.
Diagnosis
Diagnosis is the process of determining the specific medical condition or disease that is causing a patient's symptoms. It typically involves a combination of medical history, physical examination, laboratory tests, and imaging studies. Here are some common diagnostic tools and procedures:
- Medical history: A healthcare provider will ask about the patient's symptoms, medical history, and any relevant family history. This can help to identify potential risk factors and narrow down possible diagnoses.
- Physical examination: A healthcare provider will conduct a physical examination to look for signs of illness or injury. This may involve checking vital signs, listening to the heart and lungs, and examining the affected area.
- Laboratory tests: Blood tests, urine tests, and other laboratory tests can help to identify specific markers or abnormalities that may indicate a particular condition or disease.
- Imaging studies: X-rays, CT scans, MRI scans, and other imaging studies can provide detailed images of the body's internal structures, allowing healthcare providers to identify abnormalities or injuries.
- Biopsy: A biopsy involves taking a small tissue sample for examination under a microscope. This can help to identify the presence of cancer or other diseases.
Once a diagnosis has been made, healthcare providers can develop an appropriate treatment plan to manage the patient's symptoms and address the underlying condition. It's important to note that diagnosis can be complex, and some conditions may be difficult to diagnose or require multiple tests or procedures.
Treatment of slipped disc
Treatment of a slipped disc depends on the severity of the condition and the specific symptoms experienced by the patient. Here are some common treatments:
- Rest and activity modification: In mild cases, rest and avoiding activities that exacerbate symptoms can allow the body to heal the slipped disc.
- Physical therapy: A physical therapist can provide exercises to help strengthen the muscles around the spine and improve flexibility, which can help to alleviate pain and reduce the risk of future disc problems.
- Medications: Pain medications, muscle relaxants, and anti-inflammatory drugs can help to manage pain and reduce inflammation.
- Epidural injections: Steroid injections can be given directly into the spine to reduce inflammation and alleviate pain.
- Surgery: In severe cases, surgery may be necessary to remove the herniated portion of the disc and relieve pressure on the nerves.
- Alternative therapies: Acupuncture, chiropractic care, and massage therapy may be used to help alleviate pain and improve flexibility.
It's important to note that the most effective treatment for a slipped disc depends on the specific circumstances of each case. A healthcare provider can provide guidance on the most appropriate treatment options based on the severity of the condition, the patient's medical history, and other factors.
Physiotherapy treatment
Physiotherapy can be an effective treatment for a slipped disc. A physiotherapist can provide exercises and techniques to help reduce pain and improve mobility. Here are some common physiotherapy treatments for a slipped disc:
- Manual therapy: A physiotherapist can use hands-on techniques to mobilize the spine, reduce pain, and improve joint flexibility.
- Stretching and strengthening exercises: A physiotherapist can provide exercises to stretch tight muscles and strengthen weak muscles around the spine. This can help to improve posture, reduce pain, and prevent future disc problems.
- Heat and ice therapy: Heat therapy can help to relax tight muscles and improve blood flow to the affected area. Ice therapy can help to reduce inflammation and alleviate pain.
- TENS therapy: Transcutaneous electrical nerve stimulation (TENS) therapy involves applying electrical stimulation to the affected area to help reduce pain.
- Ultrasound therapy: Ultrasound therapy involves using high-frequency sound waves to reduce inflammation and improve blood flow to the affected area.
- Postural correction: A physiotherapist can provide guidance on how to improve posture and reduce strain on the spine.
- Education: A physiotherapist can provide education on how to manage symptoms and prevent future disc problems, including proper lifting techniques and exercises to maintain spinal health.
It's important to note that the most effective physiotherapy treatment for a slipped disc depends on the specific circumstances of each case. A physiotherapist can provide guidance on the most appropriate treatment options based on the severity of the condition, the patient's medical history, and other factors.
Exercises for slipped disc
Exercise can be an effective way to manage the symptoms of a slipped disc. However, it's important to note that the specific exercises recommended will depend on the severity of the condition and the specific symptoms experienced by the patient. A physiotherapist or healthcare provider can provide guidance on the most appropriate exercises for each individual case. Here are some common exercises for a slipped disc:
- Pelvic tilt: Lie on your back with your knees bent and your feet flat on the floor. Gently tilt your pelvis upward, tightening your abdominal muscles and flattening your lower back against the floor. Hold for a few seconds, then release.
- Cat-cow stretch: Begin on your hands and knees, with your wrists directly under your shoulders and your knees directly under your hips. Inhale and arch your back, lifting your head and tailbone. Exhale and round your back, tucking your chin to your chest.
- Knee-to-chest stretch: Lie on your back with your knees bent and your feet flat on the floor. Slowly bring one knee up toward your chest, holding onto your shin with your hands. Hold for 15-30 seconds, then switch legs.
- Hamstring stretch: Lie on your back with your knees bent and your feet flat on the floor. Slowly straighten one leg, lifting it toward the ceiling. Hold onto the back of your thigh with both hands, keeping your knee slightly bent. Hold for 15-30 seconds, then switch legs.
- Piriformis stretch: Lie on your back with your knees bent and your feet flat on the floor. Cross one ankle over the opposite knee, then gently pull your knee toward your opposite shoulder. Hold for 15-30 seconds, then switch legs.
- Wall sits: Stand with your back against a wall and your feet shoulder-width apart. Slowly slide down the wall until your knees are bent at a 90-degree angle. Hold for 10-20 seconds, then slowly stand back up.
It's important to note that these exercises are just a starting point and may need to be modified or adjusted depending on the specific circumstances of each case. A healthcare provider or physiotherapist can provide guidance on the most appropriate exercises and modifications based on the severity of the condition, the patient's medical history, and other factors.
How slipped disc prevented?
While it's not always possible to prevent a slipped disc, there are steps you can take to reduce your risk of developing this condition:
- Practice good posture: Maintaining good posture can help reduce the strain on your spine and prevent unnecessary pressure on your discs. Make sure to sit and stand up straight, keeping your shoulders back and your chin level.
- Exercise regularly: Regular exercise can help to strengthen the muscles around your spine, which can help to prevent disc problems. Low-impact exercises such as walking, swimming, and yoga are ideal.
- Lift heavy objects correctly: When lifting heavy objects, use your legs instead of your back to lift the weight. Bend your knees and keep your back straight, and lift the weight with your leg muscles.
- Maintain a healthy weight: Excess weight can put additional pressure on your spine, which can increase your risk of disc problems. Maintaining a healthy weight through diet and exercise can help to reduce this risk.
- Avoid repetitive activities: Repetitive activities that involve bending, twisting, or lifting can put additional strain on your spine and increase your risk of disc problems. If possible, try to avoid these activities or take frequent breaks to stretch and rest.
- Avoid smoking: Smoking can reduce blood flow to the discs in your spine, which can increase your risk of disc problems.
- Seek prompt treatment for back pain: If you experience back pain or other symptoms, seek prompt medical attention. Early treatment can help to prevent the condition from getting worse and reduce your risk of complications.
By taking these steps, you can reduce your risk of developing a slipped disc and other spine-related problems.
Conclusion
In conclusion, a slipped disc, also known as a herniated disc, is a common condition that can cause pain and discomfort in the back or neck. It occurs when a portion of a spinal disc protrudes outside its normal position, putting pressure on surrounding nerves or tissues. The condition can be caused by a variety of factors, including age, genetics, injury, and lifestyle factors.
Treatment for a slipped disc typically involves a combination of pain management, physical therapy, and exercise. However, prevention is also key, and maintaining good posture, exercising regularly, lifting heavy objects correctly, maintaining a healthy weight, avoiding repetitive activities, avoiding smoking, and seeking prompt treatment for back pain can all help to reduce the risk of developing this condition. As always, it's important to consult with a healthcare provider for personalized advice and treatment options.
No comments:
Post a Comment