What is a Posterior Pelvic Tilt?
 |
| Posterior Pelvic Tilt |
The human pelvis, a sturdy and vital structure, serves as the foundation for our entire upper body. It plays a crucial role in maintaining balance, supporting the spine, and facilitating a wide range of movements. However, when the pelvis undergoes certain misalignments, it can lead to various musculoskeletal issues and discomfort. One such misalignment is known as "Posterior Pelvic Tilt."
Defining Posterior Pelvic Tilt:
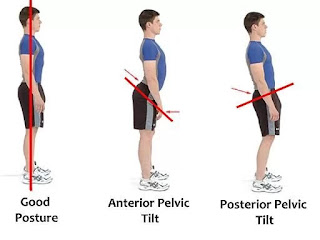
Posterior pelvic tilt, often referred to as a "tilted pelvis" or "flat back," is a condition that occurs when the top of the pelvis tilts backward, causing the lower back to flatten and the buttocks to tuck under. This alteration in the pelvic position disrupts the natural curvature of the spine and can have significant implications for an individual's overall health and well-being.
Understanding Pelvic Anatomy:
To grasp the significance of posterior pelvic tilt, it's essential to have a basic understanding of pelvic anatomy. The pelvis consists of several interconnected bones, including the ilium, ischium, pubis, and the sacrum.
These bones form a bony ring that encircles the pelvic region, with the sacrum positioned at the back. Proper alignment of these structures is crucial for maintaining stability and supporting the weight of the upper body.
The Role of Posterior Pelvic Tilt:
In a neutral or anatomically aligned pelvis, the iliac crests (the bony protrusions at the top of each hip) are approximately level horizontally, and the sacrum maintains a gentle curve. This alignment helps distribute the forces exerted on the spine evenly, reducing the risk of musculoskeletal strain.
However, when the pelvis tilts posteriorly, as seen in posterior pelvic tilt, several issues arise. The flattening of the lumbar spine puts increased pressure on the lower back, potentially leading to pain and discomfort. Additionally, the altered pelvic position affects the biomechanics of the hip joints and can result in reduced range of motion, muscle imbalances, and gait abnormalities.
In this series of articles, we will delve deeper into the various aspects of posterior pelvic tilt. We will explore its causes, symptoms, diagnosis, and most importantly, strategies for treatment and prevention. Whether you are someone dealing with the challenges of posterior pelvic tilt or a healthcare professional seeking to better understand this condition, this series aims to provide you with valuable insights and practical guidance.
So, let's embark on a journey to uncover the intricacies of posterior pelvic tilt, understand its impact on the human body, and discover effective ways to address and manage this condition for a healthier and more comfortable life.
Pelvic Anatomy and Normal Alignment:
The pelvis is a complex bony structure that serves as a critical foundation for the human body, providing support for the spine, organs, and facilitating various movements. Understanding pelvic anatomy and its normal alignment is essential for comprehending issues like pelvic tilt, injuries, and musculoskeletal conditions. Here, we will explore the components of pelvic anatomy and how they align in their typical, healthy state.
1. Pelvic Bones:
The pelvis is composed of several bones, each with a unique role in forming this essential structure:
Ilium: The large, wing-shaped bones that form the sides of the pelvis. They are often referred to as the hip bones and feature a prominent ridge called the iliac crest.
Ischium: Located at the lower and posterior part of the pelvis, the ischium bears body weight when sitting.
Pubis: The pubis bones meet at the front of the pelvis, forming the pubic symphysis, a cartilaginous joint.
Sacrum: Positioned at the back of the pelvis, the sacrum is a triangular bone formed by the fusion of several vertebrae. It connects the spine to the pelvic girdle.
2. Normal Alignment:
In a healthy and anatomically aligned pelvis, several key aspects of alignment are observed:
Iliac Crests Leveling: When looking at the pelvis from the front or back, the iliac crests on both sides should be relatively level horizontally. This means that the hips appear symmetrical.
Anterior Tilt of the Sacrum: The sacrum typically maintains a gentle anterior tilt or forward curve. This curve is a part of the natural lumbar lordosis, which contributes to the spine's S-shaped curvature.
Pubic Symphysis: The pubic symphysis at the front of the pelvis should be stable and have minimal movement. It functions as a joint with limited mobility.
Functions of the Pelvis:
The pelvis has several critical functions in the body:
Support for the Spine: The pelvis forms the base upon which the spine rests, distributing the body's weight and providing stability.
Protection for Organs: It houses and protects vital organs, including the bladder, reproductive organs, and parts of the digestive system.
Attachment for Muscles: Many muscles of the lower abdomen, hips, and thighs attach to the pelvic bones, allowing for movement and stability.
Childbirth: The pelvic shape and structure are important for childbirth, influencing the ease or difficulty of delivery.
Understanding pelvic anatomy and its normal alignment is fundamental in assessing issues like pelvic tilt or injuries. Deviations from this standard alignment can lead to various musculoskeletal problems and discomfort. In upcoming articles, we will explore conditions such as posterior pelvic tilt, anterior pelvic tilt, and ways to maintain pelvic health for overall well-being.
How it differs from anterior pelvic tilt?
Posterior pelvic tilt, also known as "pelvic retroversion" or "flat back," is a musculoskeletal condition characterized by the abnormal backward rotation of the pelvis. In posterior pelvic tilt, the top of the pelvis (the iliac crests) tilts backward or rotates posteriorly, causing the sacrum and coccyx to move in the same direction.
This results in a flattening of the natural curvature of the lumbar spine and a posterior displacement of the pelvis. As a consequence, the lower back appears flat, and the buttocks may appear tucked under or less pronounced.
Differences Between Posterior Pelvic Tilt and Anterior Pelvic Tilt:
Posterior pelvic tilt and anterior pelvic tilt are two distinct pelvic misalignments, each with its own set of characteristics and effects on the body. Here are the key differences between the two:
Direction of Pelvic Tilt:
Posterior Pelvic Tilt: In posterior pelvic tilt, the top of the pelvis tilts backward, causing the sacrum to rotate posteriorly and the lower back to flatten.
Anterior Pelvic Tilt: In anterior pelvic tilt, the top of the pelvis tilts forward, leading to an increased arch in the lower back and an anterior (forward) displacement of the pelvis. This often creates a pronounced curve in the lower back.
Appearance:
Posterior Pelvic Tilt: It can give the appearance of a flat lower back and may make the buttocks appear tucked under or less prominent.
Anterior Pelvic Tilt: It often results in an exaggerated arch in the lower back, making the buttocks and abdomen more pronounced.
Muscle Imbalances:
Posterior Pelvic Tilt: Typically involves overactive or tight hip flexor muscles and weak abdominal and gluteal muscles.
Anterior Pelvic Tilt: Often associated with overactive lumbar extensor muscles and tight lower back muscles, along with weak abdominal and hip flexor muscles.
Effects on Posture:
Posterior Pelvic Tilt: May lead to a posture where the pelvis is tilted backward, causing the upper body to lean forward.
Anterior Pelvic Tilt: Can result in a posture where the pelvis tilts forward, creating a swayback appearance with the chest pushed forward and the hips pushed backward.
Associated Symptoms:
Posterior Pelvic Tilt: Common symptoms include lower back pain, hip discomfort, and altered gait patterns.
Anterior Pelvic Tilt: Common symptoms include lower back pain, hip and knee pain, and an increased risk of postural issues.
Both posterior and anterior pelvic tilts can impact an individual's overall posture, movement, and musculoskeletal health. Treatment and management strategies may differ based on the type of pelvic tilt and its underlying causes, making it essential to accurately identify the specific pelvic alignment issue in order to provide appropriate care and rehabilitation.
Causes and risk factors for developing posterior pelvic tilt
Posterior pelvic tilt, characterized by the backward rotation of the pelvis, can result from various causes and risk factors. Understanding these factors is crucial for both prevention and effective management. Here are the primary causes and risk factors for developing posterior pelvic tilt:
1. Muscle Imbalances:
Weak Abdominal Muscles: Insufficient strength in the abdominal muscles can fail to support the pelvis properly, allowing it to tilt backward.
Weak Gluteal Muscles: The gluteal muscles, particularly the gluteus maximus, play a key role in pelvic stability. Weakness in these muscles can contribute to posterior pelvic tilt.
Tight Hip Flexors: Tightness in the hip flexor muscles, such as the iliopsoas, can pull the pelvis into a posterior tilt, especially when these muscles overpower the opposing muscle groups.
Tight Hamstrings: Tight hamstring muscles can contribute to a posterior pelvic tilt by pulling down on the back of the pelvis.
2. Poor Posture:
Prolonged Sitting: Sitting for extended periods with poor posture, especially in chairs that do not provide proper lumbar support, can encourage posterior pelvic tilt.
Slouching: Habitual slouching or rounding of the lower back can gradually lead to a posteriorly tilted pelvis.
Improper Lifting Techniques: Lifting heavy objects using incorrect techniques that place strain on the lower back can contribute to pelvic misalignment.
3. Genetics and Body Structure:
Inherent Pelvic Structure: Some individuals may have a natural pelvic structure or alignment that predisposes them to posterior pelvic tilt.
4. Gait Abnormalities:
Altered Walking Patterns: Abnormalities in the way a person walks or stands can impact pelvic alignment over time, potentially leading to posterior pelvic tilt.
5. Pregnancy:
Pregnancy-Related Changes: During pregnancy, hormonal changes and the growing uterus can affect the pelvis and may lead to temporary posterior pelvic tilt in some women.
6. Inactivity and Deconditioning:
Lack of Exercise: A sedentary lifestyle and lack of regular physical activity can result in muscle weakness and imbalances that contribute to posterior pelvic tilt.
7. Previous Injuries:
Musculoskeletal Injuries: Prior injuries to the lower back, hips, or pelvis can disrupt the normal alignment of these structures, potentially leading to posterior pelvic tilt as a compensatory mechanism.
8. Medical Conditions:
Certain Medical Conditions: Some medical conditions or musculoskeletal disorders, such as scoliosis or hip dysplasia, can influence pelvic alignment and contribute to posterior pelvic tilt.
Identifying the specific causes and risk factors that apply to an individual's case is essential for developing an effective treatment and prevention plan. Addressing muscle imbalances, improving posture, and adopting a healthy lifestyle with regular exercise can help manage and reduce the risk of developing posterior pelvic tilt. Consulting with a healthcare professional, such as a physical therapist, is advisable for a comprehensive assessment and personalized guidance.
Overview of the common symptoms associated with this condition
Posterior pelvic tilt is a musculoskeletal condition that can lead to a range of symptoms and discomfort due to the abnormal backward rotation of the pelvis. These symptoms can vary in intensity and may affect individuals differently. Here is an overview of the common symptoms associated with posterior pelvic tilt:
Lower Back Pain:
Location: Pain is typically felt in the lower back, especially in the lumbar region.
Characteristics: The pain may be dull, achy, or sharp, and it can vary in intensity.
Aggravating Factors: Activities like standing for extended periods, walking, or lifting heavy objects may exacerbate the pain.
Hip and Pelvic Discomfort:
Location: Discomfort is often experienced in the hip and pelvic region, including the sides and front of the hips.
Characteristics: It may present as a sensation of tightness, soreness, or aching.
Reduced Range of Motion:
Hip Mobility: Posterior pelvic tilt can limit the range of motion in the hip joints, making it challenging to perform certain movements like hip flexion and extension.
Spinal Mobility: The flattening of the lower back's natural curve can restrict spinal mobility, impacting activities that require bending or twisting.
Altered Gait Patterns:
Individuals with posterior pelvic tilt may exhibit changes in their walking patterns, such as a waddling gait or a tendency to lean forward slightly.
Muscle Imbalances:
Posterior pelvic tilt can lead to muscle imbalances, with certain muscles becoming overactive or tight, while others become weak or underactive.
Common imbalances include tight hip flexors and hamstrings, along with weakened abdominal and gluteal muscles.
Postural Changes:
Flat Lower Back: One of the hallmark signs of posterior pelvic tilt is a flattened or straightened lumbar spine, which can affect overall posture.
Buttock Appearance: The buttocks may appear less prominent or even tucked under in some cases.
Discomfort with Sitting and Standing:
Individuals with posterior pelvic tilt may find it uncomfortable to sit for extended periods, especially without proper lumbar support.
Standing for long durations can also be challenging and lead to discomfort.
Pain with Certain Movements:
Movements that involve lumbar extension, such as arching the back, can exacerbate lower back pain.
Bending forward or leaning backward may also trigger discomfort.
Impact on Daily Activities:
The symptoms associated with posterior pelvic tilt can affect an individual's ability to perform daily activities, including exercise, work-related tasks, and leisure activities.
It's important to note that the severity of symptoms can vary from person to person. Some individuals may experience mild discomfort, while others may have more pronounced pain and limitations in mobility. Consulting with a healthcare professional, such as a physical therapist or orthopedic specialist, is advisable for a proper evaluation and to develop an appropriate treatment plan tailored to the specific needs of the individual.
Diagnosing Posterior Pelvic Tilt
Diagnosing posterior pelvic tilt involves a comprehensive assessment by a healthcare professional, such as a physical therapist, orthopedic specialist, or chiropractor. The diagnosis typically combines a thorough physical examination, a review of medical history, and sometimes imaging studies to confirm and understand the extent of the condition. Here's an overview of the steps involved in diagnosing posterior pelvic tilt:
Medical History and Symptoms Assessment:
The healthcare provider will begin by discussing your medical history, including any past injuries, surgeries, or musculoskeletal issues.
Describe your symptoms, including the location, intensity, and duration of pain, discomfort, or mobility limitations.
Mention any relevant lifestyle factors, such as occupation, exercise routines, or recent changes in activity levels.
Physical Examination:
The healthcare provider will conduct a physical examination to assess your posture, gait, and musculoskeletal alignment.
Posture Analysis: You may be asked to stand naturally so that the provider can observe your pelvic position and spinal curvature.
Range of Motion Assessment: The provider will evaluate your ability to perform specific movements, such as hip flexion, extension, and rotation, to identify limitations or abnormalities.
Muscle Strength and Flexibility: Muscle imbalances are a common characteristic of posterior pelvic tilt. The provider will assess the strength and flexibility of key muscle groups, including the abdominals, gluteals, hip flexors, and hamstrings.
Palpation: Gentle manual palpation may be used to identify tender points, muscle tightness, or areas of discomfort around the pelvis and lower back.
Imaging Studies:
In some cases, diagnostic imaging studies may be ordered to confirm and assess the severity of posterior pelvic tilt. Common imaging modalities include:
X-rays: X-rays can provide a detailed view of the pelvic and spinal alignment, helping to measure the angle of the pelvic tilt.
MRI (Magnetic Resonance Imaging): An MRI may be used to visualize soft tissues, muscles, and any potential structural issues contributing to the condition.
Functional Assessment:
A functional assessment may involve observing how your posture and alignment change during specific movements or activities that mimic daily life or work-related tasks.
Pelvic Tilt Measurement:
The angle of pelvic tilt can be measured using X-ray images or through physical examination techniques like the inclinometer. The angle helps determine the severity of the tilt.
Differential Diagnosis:
The healthcare provider will rule out other potential causes of lower back pain or musculoskeletal issues, such as herniated discs, sciatica, or sacroiliac joint dysfunction.
Once the diagnosis is confirmed, the healthcare provider will discuss the findings with you, explain the implications of posterior pelvic tilt, and outline a treatment plan tailored to your specific needs.
Treatment may include exercises to address muscle imbalances, postural correction strategies, lifestyle modifications, and, in some cases, hands-on manual therapy.
Diagnosing posterior pelvic tilt is a critical step in addressing the condition effectively. A healthcare professional's expertise and a thorough assessment ensure that the treatment plan is tailored to your unique circumstances and helps you achieve improved pelvic alignment and overall musculoskeletal health.
Treating Posterior Pelvic Tilt
Treating posterior pelvic tilt involves a multifaceted approach that addresses muscle imbalances, postural issues, and lifestyle factors contributing to the condition. The goal is to restore proper pelvic alignment, alleviate pain and discomfort, and prevent the recurrence of the tilt. Here are the key components of treating posterior pelvic tilt:
Physical Therapy and Exercise:
A physical therapist will design a customized exercise program to address muscle imbalances associated with posterior pelvic tilt.
Strengthening Weak Muscles: Emphasis is placed on strengthening the abdominal muscles, particularly the transverse abdominis, as well as the gluteal muscles (especially the gluteus maximus).
Stretching Tight Muscles: Targeted stretching exercises are prescribed to release tight hip flexors, hamstrings, and lower back muscles.
Core Stability Training: Core strengthening exercises help improve stability and support for the pelvis and lower back.
Postural Correction:
Education: Learning about proper posture and ergonomic principles is essential. Individuals with posterior pelvic tilt should be mindful of their posture during daily activities and work.
Postural Exercises: Specific exercises and techniques are taught to help maintain a neutral pelvis and spine alignment.
Manual Therapy:
Some individuals may benefit from hands-on manual therapy techniques provided by a physical therapist or chiropractor. These techniques may include joint mobilization, myofascial release, and soft tissue manipulation to improve mobility and reduce muscle tension.
Ergonomic Adjustments:
Making adjustments to workstations, chairs, and the environment can help support a neutral pelvis and reduce strain on the lower back.
Ergonomic assessments and recommendations may be provided by specialists.
Lifestyle Modifications:
Weight Management: Maintaining a healthy weight can alleviate excess stress on the lower back and pelvis.
Avoiding Prolonged Sitting: Frequent breaks, standing desks, or ergonomic chairs can help reduce the negative effects of prolonged sitting.
Proper Lifting Techniques: Learning and practicing safe lifting techniques can prevent additional strain on the lower back.
Bracing and Support:
In some cases, a brace or support belt may be recommended to help maintain pelvic alignment, particularly during activities that may exacerbate the condition.
Patient Education:
Understanding the condition and its contributing factors is crucial. Patients should be educated on the importance of exercise, posture, and self-care practices.
Monitoring and Follow-Up:
Regular check-ins with a healthcare provider, physical therapist, or chiropractor are essential to track progress and make necessary adjustments to the treatment plan.
Surgical Intervention (Rare):
Surgery is generally considered a last resort and is reserved for cases of severe pelvic tilt caused by structural issues that do not respond to conservative treatments.
It's important to note that the effectiveness of treatment for posterior pelvic tilt varies depending on the individual's unique circumstances, including the severity of the condition and adherence to the prescribed treatment plan. Early intervention and consistent self-care practices can significantly improve outcomes and help individuals manage and potentially resolve posterior pelvic tilt. Consulting with a healthcare professional is crucial for developing a personalized treatment plan tailored to your needs.
Physiotherapy Treatment
Physiotherapy, also known as physical therapy, plays a crucial role in the treatment of posterior pelvic tilt. A physical therapist is trained to assess and address musculoskeletal issues, including muscle imbalances and postural problems that contribute to this condition. Here's how physiotherapy treatment can help manage and correct posterior pelvic tilt:
1. Assessment and Diagnosis:
The first step in physiotherapy treatment is a thorough assessment to determine the extent of posterior pelvic tilt and identify any underlying causes, such as muscle imbalances or structural issues.
2. Individualized Exercise Programs:
Physical therapists design customized exercise programs tailored to the individual's specific needs and goals.
Exercises focus on strengthening weak muscles, particularly the abdominal and gluteal muscles, and stretching tight muscles such as the hip flexors and hamstrings.
Core stability exercises are essential for improving pelvic stability and spinal alignment.
3. Manual Therapy Techniques:
Hands-on manual therapy techniques, such as joint mobilization, soft tissue massage, and myofascial release, can be used to improve joint mobility and reduce muscle tension.
4. Postural Correction:
Education on proper posture is a fundamental component of physiotherapy treatment.
Patients are taught how to maintain a neutral pelvis and spine during daily activities, work, and exercise.
Specific postural exercises and techniques are prescribed to reinforce proper alignment.
5. Gait Analysis:
In some cases, gait analysis may be conducted to assess walking patterns and identify abnormalities related to posterior pelvic tilt.
Based on the analysis, modifications may be recommended to improve gait mechanics.
6. Ergonomic Advice:
Physical therapists can provide guidance on ergonomics in the workplace and at home to reduce stress on the lower back and pelvis.
This may include recommendations for workstation setup, chair selection, and lifting techniques.
7. Functional Rehabilitation:
Functional exercises that mimic daily activities are integrated into the treatment plan to help individuals regain the ability to perform tasks without pain or discomfort.
8. Monitoring and Progression:
Physical therapists monitor progress throughout the treatment process and make adjustments to exercise programs as needed.
Patients are educated on self-management techniques to maintain and continue their progress independently.
9. Patient Education:
Education about the condition, its causes, and strategies for prevention is an integral part of physiotherapy treatment.
Patients are empowered to take an active role in their recovery and long-term musculoskeletal health.
10. Follow-Up and Maintenance:
Physiotherapy treatment for posterior pelvic tilt is typically a conservative and non-invasive approach. In the majority of cases, with consistent adherence to the prescribed exercises and lifestyle modifications, individuals can experience significant improvements in pelvic alignment, reduced pain, and enhanced function. However, it's crucial to consult with a qualified physical therapist for a comprehensive assessment and personalized treatment plan tailored to your specific needs and condition.
Stretching Exercise
Stretching exercises play a vital role in the treatment and management of posterior pelvic tilt. They help alleviate muscle tightness and improve flexibility, particularly in the hip flexors, hamstrings, and lower back muscles. Here are some stretching exercises that can be beneficial for individuals with posterior pelvic tilt:
Hip Flexor Stretch:
Kneel on one knee and extend the other leg in front of you.
Tilt your pelvis forward slightly by engaging your glutes.
Gently lean forward, keeping your back straight, until you feel a stretch in the front of the hip on the kneeling leg.
Hold the stretch for 20-30 seconds, and repeat on the other side.
Perform 2-3 sets on each side.
Hamstring Stretch:
Sit on the floor with one leg extended straight and the other leg bent so that the sole of your foot is against the inner thigh of your extended leg.
Keeping your back straight, hinge at the hips and reach toward your toes.
Hold the stretch for 20-30 seconds, feeling the stretch along the back of your extended leg.
Repeat on the other side and perform 2-3 sets on each side.
Child's Pose:
Begin on your hands and knees in a tabletop position.
Sit back on your heels, extending your arms forward and lowering your chest toward the floor.
Keep your hips resting on your heels and your arms extended as far as comfortable.
Hold the stretch for 20-30 seconds, feeling a gentle stretch in your lower back and hips.
Cat-Cow Stretch:
Start in a tabletop position with your hands under your shoulders and knees under your hips.
Inhale, arching your back, lifting your head and tailbone (Cow Pose).
Exhale, rounding your back, tucking your chin, and tucking your pelvis (Cat Pose).
Flow between these two positions, inhaling and exhaling with each movement, for 30 seconds.
Seated Forward Bend:
Sit with your legs extended straight in front of you.
Keeping your back straight, hinge at the hips and reach for your toes.
Hold the stretch for 20-30 seconds, feeling the stretch along your hamstrings and lower back.
Quad Stretch:
Stand with feet hip-width apart.
Bend one knee and bring your heel toward your buttocks.
Reach back with the same-side hand to hold your ankle or foot.
Gently pull your heel towards your buttocks while keeping your knees close together.
Hold for 20-30 seconds and repeat on the other leg.
Piriformis Stretch:
Sit on the floor with both legs extended.
Cross one leg over the other, placing the ankle on the opposite thigh.
Gently press down on the knee of the crossed leg until you feel a stretch in the buttock area.
Hold for 20-30 seconds and switch to the other leg.
Perform these stretching exercises regularly, aiming for consistency rather than intensity. Stretching can help improve flexibility, reduce muscle tightness, and promote better pelvic alignment, which is beneficial for managing posterior pelvic tilt. If you have any specific medical concerns or conditions, consult with a healthcare provider or physical therapist before starting a new exercise routine.
Strengthening Exercise
Strengthening exercises are an essential component of managing and correcting posterior pelvic tilt. These exercises target key muscle groups, including the abdominals, gluteals, and lower back, to improve pelvic stability and restore proper alignment. Here are some effective strengthening exercises for individuals with posterior pelvic tilt:
1. Pelvic Tilt Exercise:
Lie on your back with your knees bent and feet flat on the floor, hip-width apart.
Place your hands on your lower abdomen or pelvis.
Inhale, then exhale as you gently tilt your pelvis backward, flattening your lower back against the floor.
Hold this position for a few seconds, maintaining engagement in your lower abdominals.
Inhale and return to the neutral position.
Perform 10-15 repetitions for 2-3 sets.
2. Bird-Dog Exercise:
Begin on your hands and knees in a tabletop position.
Extend your right arm forward while simultaneously extending your left leg straight back.
Keep your spine in a neutral position and your pelvis level.
Hold for a few seconds, then return to the starting position.
Repeat with your left arm and right leg.
Perform 10-12 repetitions on each side for 2-3 sets.
3. Glute Bridges:
Lie on your back with your knees bent and feet flat on the floor, hip-width apart.
Place your arms by your sides, palms facing down.
Engage your gluteal muscles and lift your hips off the ground, creating a straight line from your shoulders to your knees.
Hold the bridge position for a few seconds, then lower your hips back down.
Perform 12-15 repetitions for 2-3 sets.
4. Clamshells:
Lie on your side with your legs bent at a 90-degree angle and your feet together.
Keep your feet touching and open your top knee as far as comfortably possible while maintaining the alignment of your pelvis.
Hold the open position for a few seconds, then close your knee back down.
Perform 12-15 repetitions on each side for 2-3 sets.
5. Planks:
Start in a push-up position with your elbows directly under your shoulders and your toes on the ground.
Keep your body in a straight line from head to heels, engaging your core muscles.
Hold this position for 20-30 seconds (or longer as you progress).
Repeat for 2-3 sets.
6. Side Planks:
Lie on your side with your legs extended and feet stacked on top of each other.
Prop yourself up on your elbow directly under your shoulder.
Lift your hips off the ground, creating a straight line from head to heels.
Hold for 20-30 seconds on each side for 2-3 sets.
7. Dead Bugs:
Lie on your back with your arms extended toward the ceiling and your knees bent at a 90-degree angle.
Lower your right arm and left leg toward the floor while keeping your lower back pressed into the ground.
Return to the starting position and repeat with the opposite arm and leg.
Perform 10-12 repetitions on each side for 2-3 sets.
These strengthening exercises help improve muscle balance, support pelvic stability, and promote proper alignment. Start with an appropriate number of repetitions and sets, and gradually increase the intensity as your strength and endurance improve. Always maintain proper form during these exercises to ensure their effectiveness and minimize the risk of injury. If you're unsure about the suitability of these exercises for your condition, consult with a physical therapist or healthcare provider for guidance.
Complications
Posterior pelvic tilt, if left untreated or unmanaged, can lead to several complications and secondary issues that can affect an individual's musculoskeletal health and overall well-being. It's essential to address and manage posterior pelvic tilt to prevent or mitigate these potential complications. Here are some of the possible complications associated with posterior pelvic tilt:
Chronic Lower Back Pain: One of the most common complications of posterior pelvic tilt is chronic lower back pain. The flattening of the lumbar spine and altered pelvic alignment can place excessive strain on the lower back muscles and structures, leading to ongoing discomfort and pain.
Muscle Imbalances: Posterior pelvic tilt is often associated with muscle imbalances, such as weak abdominal and gluteal muscles and tight hip flexors and hamstrings. These imbalances can contribute to gait abnormalities, altered movement patterns, and an increased risk of injuries.
Reduced Mobility: Posterior pelvic tilt can restrict the range of motion in the hip joints and lumbar spine. This reduced mobility can limit an individual's ability to perform activities of daily living and lead to stiffness and discomfort.
Postural Issues: Prolonged posterior pelvic tilt can contribute to poor posture. Individuals may adopt a posture where the pelvis is tilted backward, causing the upper body to lean forward. This posture can lead to further musculoskeletal issues and discomfort.
Degenerative Changes: Chronic misalignment of the pelvis and lumbar spine can contribute to degenerative changes in the spine, such as early disc degeneration or facet joint arthrosis. These changes can result in long-term pain and reduced spinal function.
Reduced Quality of Life: Persistent pain, limited mobility, and compromised musculoskeletal health can have a significant impact on an individual's quality of life. Everyday activities, work, and leisure pursuits may become more challenging and less enjoyable.
Psychosocial Impact: Living with chronic pain and physical limitations can lead to emotional and psychological stress, anxiety, and depression. These psychosocial factors can further exacerbate the perception of pain and disability.
Compensatory Mechanisms: To cope with posterior pelvic tilt, the body may develop compensatory mechanisms that can lead to additional musculoskeletal issues. For example, an individual might unconsciously overuse certain muscle groups or adapt their gait in a way that places stress on other joints.
Reduced Athletic Performance: Athletes with posterior pelvic tilt may experience a decline in athletic performance due to compromised biomechanics, muscle imbalances, and increased susceptibility to injuries.
It's important to address posterior pelvic tilt through a combination of physical therapy, exercise, posture correction, and lifestyle modifications. Early intervention and proactive management can help prevent these complications or reduce their severity. Consulting with a healthcare professional, such as a physical therapist or orthopedic specialist, is crucial to develop a personalized treatment plan and prevent the potential complications associated with posterior pelvic tilt.
How to Prevent Posterior Pelvic Tilt?
Preventing posterior pelvic tilt involves a combination of lifestyle adjustments, exercise routines, and ergonomic considerations aimed at maintaining proper pelvic alignment and overall musculoskeletal health. Here are some strategies to help prevent posterior pelvic tilt:
Maintain a Strong Core:
Strengthen your core muscles, including the transverse abdominis and obliques, through targeted exercises. A strong core provides stability to the pelvis and helps maintain proper alignment.
Focus on Hip and Gluteal Strength:
Engage in exercises that strengthen the gluteus maximus and medius, as well as the hip abductors and external rotators. These muscles play a crucial role in stabilizing the pelvis.
Stretch Regularly:
Incorporate stretching exercises to maintain flexibility in the hip flexors, hamstrings, and lower back. Stretching helps prevent muscle tightness and imbalances.
Practice Good Posture:
Pay attention to your posture, whether sitting, standing, or walking. Avoid slouching, and aim to keep your pelvis in a neutral position.
Ergonomic Workspace Setup:
If you have a desk job, set up an ergonomic workstation. Use an adjustable chair with lumbar support and ensure your computer monitor is at eye level. Take regular breaks to stand and move around.
Lift Properly:
When lifting heavy objects, use proper lifting techniques. Bend at the hips and knees, not the waist, and engage your core muscles. Keep the object close to your body as you lift.
Incorporate Pelvic Tilt Exercises:
Include exercises like pelvic tilts in your routine to improve awareness of your pelvic position. These exercises can help maintain a neutral pelvis and prevent excessive tilt.
Stay Active:
Engage in regular physical activity to maintain overall strength, flexibility, and mobility. Activities like swimming, yoga, and Pilates can be particularly beneficial.
Avoid Prolonged Sitting:
If your work or lifestyle involves long periods of sitting, take breaks to stand, stretch, and walk around. Consider using a standing desk or sit-stand workstation.
Stay Hydrated:
Proper hydration is essential for maintaining muscle and joint health. Dehydration can contribute to muscle cramps and tightness.
Maintain a Healthy Weight:
Excess weight can put additional stress on the pelvis and lower back. Maintaining a healthy weight can reduce the risk of developing musculoskeletal issues.
Regular Check-Ups:
Schedule regular check-ups with a healthcare provider or physical therapist to assess your musculoskeletal health and receive guidance on preventive measures.
Listen to Your Body:
Pay attention to any signs of discomfort or pain in the lower back or pelvis. Early awareness of issues can lead to prompt intervention and prevention of further problems.
Footwear Considerations:
Choose supportive shoes with proper arch support and cushioning, especially if you spend a lot of time on your feet.
Educate Yourself:
Learn about proper body mechanics, ergonomics, and posture through educational resources or consultations with healthcare professionals.
Preventing posterior pelvic tilt involves a proactive approach to musculoskeletal health. By incorporating these strategies into your daily life, you can reduce the risk of developing this condition and maintain better overall pelvic alignment and posture. If you have specific concerns or are already experiencing symptoms of posterior pelvic tilt, consult with a healthcare provider or physical therapist for personalized guidance and interventions.
Conclusion
In conclusion, posterior pelvic tilt is a musculoskeletal condition characterized by the backward rotation of the pelvis, leading to a flattening of the lumbar spine and potential musculoskeletal imbalances. It can result from various factors, including muscle weaknesses, poor posture, genetics, and lifestyle choices. However, with proper diagnosis and management, individuals can effectively address and prevent the associated complications.
Treatment for posterior pelvic tilt typically includes physical therapy, exercises to strengthen and stretch specific muscle groups, postural correction, ergonomic adjustments, and lifestyle modifications. These interventions aim to improve pelvic stability, alleviate pain, and restore proper pelvic alignment.
Preventing posterior pelvic tilt involves maintaining a strong core, hip, and gluteal muscles, practicing good posture, setting up ergonomic workspaces, lifting objects correctly, staying active, and being mindful of your body's signals. Regular check-ups with healthcare professionals can also help you stay on top of your musculoskeletal health.
Overall, by adopting a proactive approach to musculoskeletal health and following the guidance of healthcare professionals, individuals can manage and prevent posterior pelvic tilt, leading to improved well-being and a higher quality of life.

