What is an Ankylosing Spondylitis?
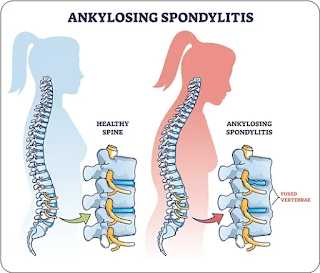
Ankylosing spondylitis (AS) is a type of inflammatory arthritis that primarily affects the spine, but can also affect other joints and organs. It belongs to a group of conditions known as spondyloarthropathies, which involve inflammation of the joints and connective tissues.
AS typically starts with inflammation in the sacroiliac joints, which are located where the lower spine meets the pelvis. This can cause pain and stiffness in the lower back, hips, and buttocks. Over time, the inflammation can spread to other parts of the spine and other joints, causing pain, stiffness, and loss of mobility.
Other symptoms of AS may include fatigue, fever, loss of appetite, and weight loss. In severe cases, AS can cause spinal deformity and lead to compression of the spinal cord or nerve roots, which can result in neurological complications.
AS is a chronic condition that tends to develop slowly over time. It usually affects people in their late teens or early twenties and is more common in men than women. There is no cure for AS, but treatment can help manage symptoms and prevent complications. Treatment may include medications to reduce inflammation, physical therapy, and surgery in severe cases.
What are the Symptoms of Ankylosing Spondylitis?
The symptoms of ankylosing spondylitis (AS) can vary from person to person, but they usually involve pain and stiffness in the lower back, hips, and buttocks. Other symptoms may include:
- Pain and stiffness in other joints, such as the knees, ankles, and shoulders
- Fatigue and a general feeling of being unwell
- Inflammation and pain in the eyes (uveitis)
- Difficulty taking deep breaths or expanding the chest wall
- Reduced flexibility and range of motion in the spine and other joints
- Pain in the heels or bottom of the feet due to inflammation where the tendons attach to the bone
- Loss of appetite and weight loss
Symptoms of AS tend to develop slowly over time and may come and go. They may also be more severe in the morning or after periods of inactivity. In some cases, AS can cause complications such as spinal fractures, compression of the spinal cord, or problems with the heart, lungs, and eyes.
Causes of Ankylosing Spondylitis
The exact cause of ankylosing spondylitis (AS) is not yet fully understood, but it is believed to be a combination of genetic and environmental factors.
- Genetic Factors: A particular gene called HLA-B27 has been strongly associated with the development of AS. However, not everyone with this gene develops AS, and not everyone with AS has this gene.
- Environmental Factors: Some environmental factors have also been linked to the development of AS, including infections, such as bacterial or viral infections, and exposure to certain toxins.
- Autoimmune Factors: AS is classified as an autoimmune disease, which means that the body's immune system mistakenly attacks its own tissues, causing inflammation and damage. In AS, the immune system attacks the joints in the spine and other parts of the body.
- Family History: AS can run in families, indicating a genetic predisposition.
It is important to note that while AS cannot be cured, early diagnosis and treatment can help manage symptoms and prevent further complications.
Complications of Ankylosing Spondylitis
Ankylosing spondylitis (AS) can cause several complications if left untreated or if it is not managed properly. Some of the possible complications include:
- Spinal deformities: AS can cause the bones of the spine to fuse together, resulting in a rigid and inflexible spine that can lead to a hunched posture or curvature of the spine (kyphosis).
- Fractures: AS can increase the risk of spinal fractures, especially if the spine has become rigid and brittle due to the fusion of the bones.
- Eye inflammation: Some people with AS can develop inflammation in the eyes (uveitis), which can cause eye pain, redness, and sensitivity to light.
- Heart and lung problems: In rare cases, AS can cause inflammation in the heart or lungs, leading to heart and lung problems.
- Neurological complications: Severe spinal deformities can lead to compression of the spinal cord or nerve roots, resulting in neurological complications such as numbness, weakness, or tingling in the limbs, or problems with bladder and bowel function.
- Osteoporosis: Chronic inflammation and long-term use of corticosteroids to manage AS can increase the risk of osteoporosis, a condition in which the bones become weak and brittle.
It is important for people with AS to work closely with their healthcare providers to manage their symptoms and prevent complications.
Risk factor
There are several factors that can increase a person's risk of developing ankylosing spondylitis (AS), including:
- Genetics: AS has a strong genetic component, and having a family history of AS increases the risk of developing the condition.
- Age and gender: AS usually develops in late adolescence or early adulthood, and is more common in men than in women.
- Ethnicity: AS is more common in people of certain ethnic backgrounds, including Caucasians and Asians.
- HLA-B27 gene: The presence of the HLA-B27 gene is strongly associated with the development of AS, although not everyone with the gene develops the condition, and not everyone with AS has the gene.
- Infections: Certain bacterial and viral infections have been linked to the development of AS, although the exact relationship between infections and AS is not yet fully understood.
- Environmental factors: Exposure to certain environmental factors, such as smoking and pollution, may increase the risk of developing AS.
It is important to note that having one or more of these risk factors does not necessarily mean that a person will develop AS, and many people with AS do not have any known risk factors.
Differential Diagnosis
Ankylosing spondylitis (AS) shares some symptoms with other conditions, so it is important to consider a few differential diagnoses when assessing a patient suspected of having AS. Some of the conditions that may be confused with AS include:
- Mechanical back pain: Back pain due to muscle strains, ligament sprains, or other mechanical causes can resemble AS, but it typically responds to rest and physical therapy rather than medication.
- Osteoarthritis: Osteoarthritis is a degenerative joint disease that can cause pain and stiffness in the joints, including the spine.
- Unlike AS, osteoarthritis usually affects older adults and does not cause the same degree of inflammation.
- Psoriatic arthritis: Psoriatic arthritis is a type of arthritis that occurs in people with psoriasis, a skin condition. Like AS, it can cause joint pain, stiffness, and inflammation, but it can also affect the hands and feet and cause skin changes.
- Reactive arthritis: Reactive arthritis is a type of arthritis that occurs in response to an infection in another part of the body, such as the gastrointestinal tract or the genital area. It can cause joint pain and inflammation, especially in the lower extremities.
- Inflammatory bowel disease (IBD)-associated arthritis: Arthritis can occur as a complication of inflammatory bowel diseases (IBD), such as Crohn's disease or ulcerative colitis. This type of arthritis typically affects the peripheral joints, such as the knees, ankles, and wrists.
It is important to seek medical attention if you are experiencing any symptoms of AS or any other condition so that your healthcare provider can perform a thorough evaluation and make an accurate diagnosis.
Diagnosis
The diagnosis of ankylosing spondylitis (AS) typically involves a combination of medical history, physical examination, and imaging tests. The process may include the following:
- Medical history: The healthcare provider will ask about symptoms, family history of AS, and any other medical conditions or medications that could be contributing to the symptoms.
- Physical examination: The healthcare provider will perform a physical exam to check for signs of inflammation and stiffness in the joints, especially in the spine and sacroiliac joints (where the spine meets the pelvis).
- Blood tests: Blood tests can help to detect inflammation in the body and rule out other conditions that may have similar symptoms.
- Imaging tests: X-rays and magnetic resonance imaging (MRI) scans can show changes in the spine and sacroiliac joints that are consistent with AS, such as bone spurs, a fusion of the vertebrae, and inflammation.
- HLA-B27 testing: A blood test can be done to detect the presence of the HLA-B27 gene, which is strongly associated with the development of AS.
- Assessment of disease activity and functional limitations: Several tools are available to assess the severity of the disease, including the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and the Bath Ankylosing Spondylitis Functional Index (BASFI).
It is important to note that AS can be a difficult condition to diagnose, as its symptoms can mimic those of other conditions. It may take some time to reach a definitive diagnosis, and patients may be referred to a specialist, such as a rheumatologist, for further evaluation and management.
Treatment of Ankylosing Spondylitis
There is currently no cure for ankylosing spondylitis (AS), but there are several treatments that can help to manage symptoms and slow the progression of the disease. Treatment options may include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs, such as ibuprofen and naproxen, can help to reduce pain and inflammation in the joints.
- Disease-modifying antirheumatic drugs (DMARDs): DMARDs, such as sulfasalazine, can help to slow the progression of the disease and reduce inflammation.
- Biologic medications: Biologic medications, such as tumor necrosis factor (TNF) inhibitors, can help to reduce inflammation and slow the progression of the disease in people with more severe symptoms.
- Physical therapy: Physical therapy can help to improve mobility, strength, and flexibility, and reduce pain and stiffness.
- Exercise: Regular exercise can help to maintain joint mobility and reduce pain and stiffness, but it is important to work with a healthcare provider or physical therapist to develop a safe and effective exercise plan.
- Surgery: In rare cases, surgery may be recommended to correct severe joint damage or spinal deformities.
- If you are looking for Physiotherapy treatment, you can contact us at our clinic.
It is important to work closely with a healthcare provider to develop an individualized treatment plan that addresses your specific symptoms and needs. Regular monitoring and follow-up appointments may be necessary to adjust treatment as needed and ensure that the disease is well-managed.
Exercise for Ankylosing Spondylitis
Exercise can be an important part of the management of ankylosing spondylitis (AS), as it can help to maintain joint mobility, improve posture, and reduce pain and stiffness. However, it is important to work with a healthcare provider or physical therapist to develop a safe and effective exercise plan that takes into account your specific symptoms and limitations.
Here are some types of exercises that may be beneficial for people with AS:
- Range-of-motion exercises: These exercises involve moving the joints through their full range of motion, and can help to maintain flexibility and mobility in the spine and other affected joints.
- Strengthening exercises: Strengthening exercises can help to improve muscle strength and reduce stress on the joints.
- Exercises that target the muscles of the back, hips, and legs may be especially beneficial for people with AS.
- Aerobic exercises: Aerobic exercises, such as walking, swimming, or cycling, can help to improve cardiovascular fitness and overall health. Low-impact exercises are usually recommended to reduce stress on the joints.
- Stretching exercises: Stretching exercises can help to improve flexibility and reduce muscle tension, which can help to reduce pain and stiffness. Gentle stretching exercises for the back, hips, and legs may be beneficial for people with AS.
- Yoga or Pilates: These forms of exercise can help to improve flexibility, strength, and posture, and may also promote relaxation and stress reduction.
It is important to start exercise gradually and build up slowly, to avoid overexertion and injury. It is also important to avoid exercises that involve sudden, jerking movements or high-impact activities that can put stress on the joints. Working with a healthcare provider or physical therapist can help to develop a safe and effective exercise plan that is tailored to your specific needs and limitations.
How Ankylosing Spondylitis prevented?
There is no known way to prevent ankylosing spondylitis (AS) since it is a genetic condition. However, there are steps that individuals with a family history of AS can take to reduce their risk of developing the condition or experiencing severe symptoms:
Early diagnosis and treatment: Early diagnosis and treatment can help to manage symptoms and slow the progression of the disease. If you have a family history of AS or are experiencing symptoms, talk to your healthcare provider about getting screened for the condition.
Regular exercise: Regular exercise can help to maintain joint mobility, improve posture, and reduce pain and stiffness. It is important to work with a healthcare provider or physical therapist to develop a safe and effective exercise plan.
Good posture: Maintaining good posture can help to reduce stress on the spine and other joints. Avoid slouching or hunching over, and use ergonomic equipment, such as an adjustable chair and keyboard, if you work at a desk.
Quit smoking: Smoking has been shown to increase the risk of developing AS and may worsen symptoms in people who already have the condition. Quitting smoking can help to reduce this risk.
Maintain a healthy weight: Excess weight can put stress on the joints and worsen symptoms. Maintaining a healthy weight through a balanced diet and regular exercise can help to reduce this stress.
It is important to note that AS can be a complex and unpredictable condition and that some individuals with a family history of the condition may still develop it despite taking preventative measures. Regular monitoring and follow-up with a healthcare provider can help to ensure that the condition is well-managed and complications are prevented or minimized.
Prognosis
The prognosis for ankylosing spondylitis (AS) varies widely depending on the severity of the disease and how well it is managed.
In some cases, the disease may progress slowly and cause relatively mild symptoms, while in other cases, it may progress more rapidly and cause more severe symptoms and complications.
In general, early diagnosis and treatment can help to slow the progression of the disease and improve long-term outcomes.
Regular monitoring and follow-up with a healthcare provider can help to ensure that the disease is well-managed and complications are prevented or minimized.
Complications of AS, such as spinal deformities or damage to other joints, can have a significant impact on quality of life and mobility. However, with appropriate treatment and management, many people with AS are able to maintain good function and quality of life.
It is important to note that AS is a chronic condition that requires ongoing management and care. With proper treatment and self-care, many people with AS are able to live full and active lives.
Conclusion
Ankylosing spondylitis (AS) is a chronic inflammatory condition that primarily affects the spine and can lead to pain, stiffness, and reduced mobility. It is a genetic condition, so there is no known way to prevent it, but early diagnosis and treatment can help to manage symptoms and slow the progression of the disease.
Treatment options for AS may include medication, physical therapy, and exercise, and it is important to work with a healthcare provider to develop a treatment plan that is tailored to your specific needs and symptoms. Regular monitoring and follow-up with a healthcare provider can help to ensure that the disease is well-managed and complications are prevented or minimized.
Although AS can be a complex and unpredictable condition, with appropriate treatment and self-care, many people with AS are able to maintain good function and quality of life.
No comments:
Post a Comment